New COVID Variant ‘Nimbus’ Spreads Fast Across U.S.: As we move into summer 2025, a new COVID-19 variant is grabbing national attention: NB.1.8.1, better known by its catchy nickname—“Nimbus.” First identified earlier this year, this fast-moving Omicron subvariant is now responsible for a growing share of infections across the United States. From Los Angeles to tribal communities in Arizona, and even as far as Alaska and the Great Plains, health officials are tracking a noticeable increase in both positive tests and symptomatic illness.
The name Nimbus might sound whimsical (yes, it’s a nod to Harry Potter), but its spread is no laughing matter. Characterized by a “razor-blade throat” and high transmissibility, Nimbus has gone from a curiosity to a top U.S. variant in just a few months. With COVID fatigue setting in and vaccination rates plateauing, many Americans are wondering: Do we need to worry? Is this another wave? Should I mask again? In this article, we’ll break it all down—what Nimbus is, how it compares to other variants, what symptoms to look for, and most importantly, what actions you can take to protect yourself, your family, and your community this summer. Whether you’re a parent, healthcare worker, business owner, or tribal elder, these facts are for you—no jargon, just truth.

New COVID Variant ‘Nimbus’ Spreads Fast Across U.S.
Let’s be real: by this point in the pandemic, most of us are done with COVID—but unfortunately, COVID isn’t done with us. Variants like Nimbus (NB.1.8.1) are a reminder that the virus continues to evolve, even if our patience doesn’t. The good news? We’re not where we were in 2020—or even 2022. We’ve got tools: vaccines, boosters, testing, treatments, and knowledge. That’s power, if we choose to use it.
So, what’s the call to action here?
- Don’t ignore symptoms just because they seem “mild” or common. That sore throat could be Nimbus.
- Stay up to date on your boosters. Immunity wanes faster than most people realize—especially against fast-spreading variants.
- Support vulnerable folks—immunocompromised people, elders, frontline workers—by masking indoors and isolating when sick.
- Check in with your local health departments or tribal health services to stay informed. These teams are doing the groundwork to protect communities and need your cooperation.
If you’re a professional—doctor, nurse, educator, or community leader—your guidance and influence matter more than ever. Clear communication builds trust. And trust saves lives.
This isn’t about panic. It’s about being prepared. It’s about making small, smart decisions that allow us to enjoy summer gatherings, powwows, graduations, and family cookouts—safely.
So yes, the Nimbus variant is spreading fast. But we’ve got the knowledge, the tools, and the community strength to weather it together. Let’s not wait for a surge to start caring. Let’s act now, stay connected, and protect each other.
| Topic | Details |
|---|---|
| Variant Name | NB.1.8.1 (nicknamed Nimbus) |
| Nicknamed For | Quidditch vacuum Nimbus 2000—fast as a broomstick |
| First Detected | January 2025 globally; widespread by May |
| WHO Status | Variant Under Monitoring (May 23, 2025) – WHO |
| US Prevalence | ~37% of sequenced cases by June 2025 |
| Main Symptom | Razor‑blade throat – extremely sore |
| Other Symptoms | Cough, congestion, fatigue, fever, nausea |
| Risk Level | Still Low – no increase in severity |
| Vaccine Protection | ~1.6× reduction in antibody effectiveness, but still protects |
| CDC Page | CDC – COVID Variant Info |
What Is the Nimbus Variant?
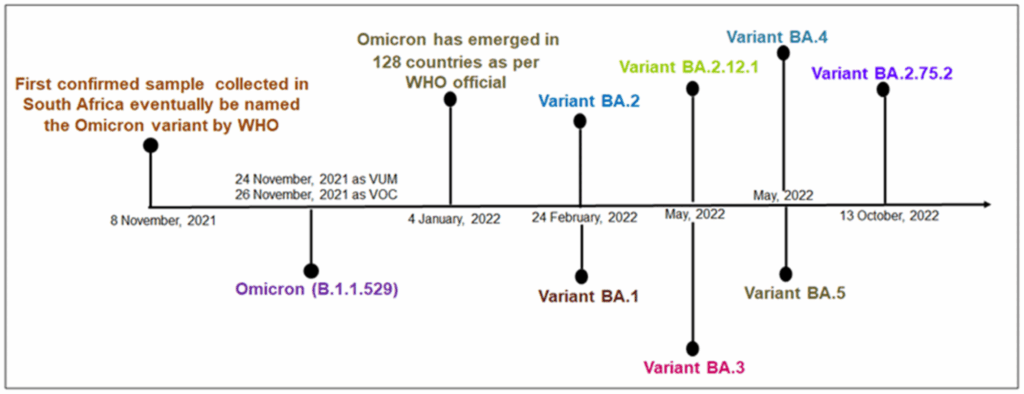
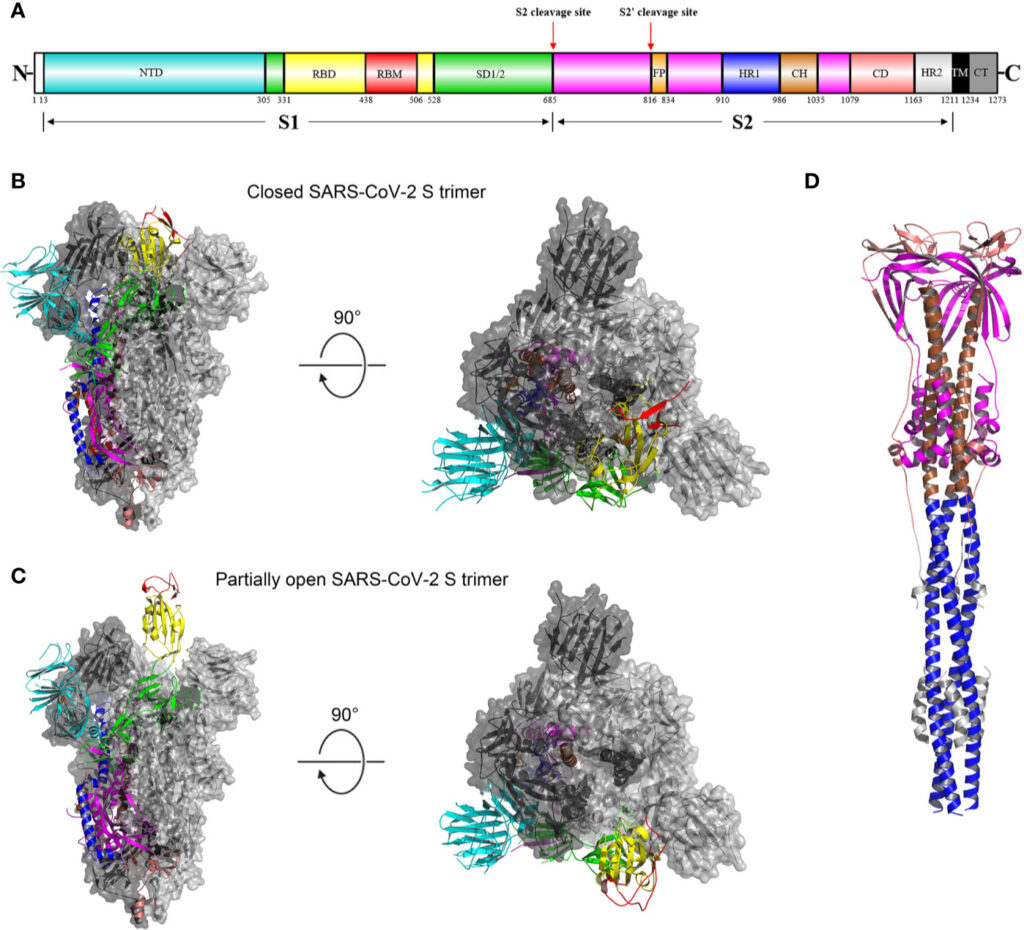
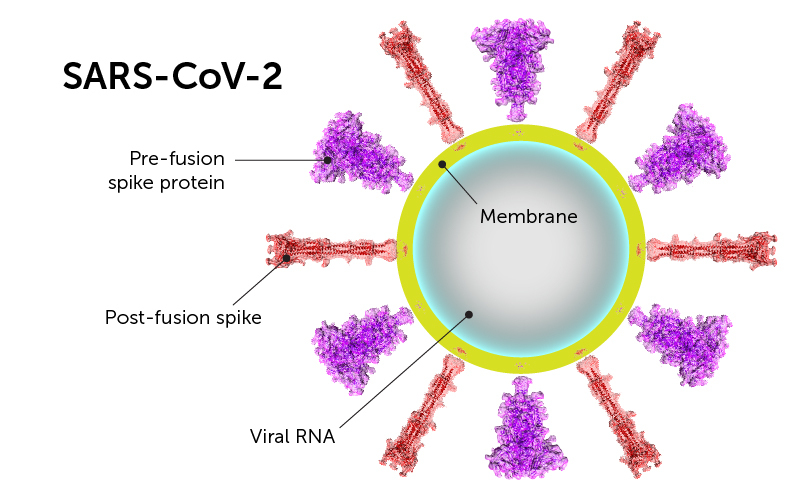
The Nimbus variant, officially NB.1.8.1, stems from the Omicron family—yes, the same cousin responsible for waves in 2021–22. It’s a recombinant strain: two Omicron versions shuffled genetic material, resulting in about 27 mutations, including 7 on the spike protein—the part of the virus that latches onto human cells.
Why the name Nimbus? Think of the fast-moving Nimbus 2000 broom in Harry Potter. When lab data showed how quickly NB.1.8.1 spreads, citizen-scientists and social media users coined the nickname—easy to remember and relatable.
New COVID Variant ‘Nimbus’ Spreads Fast Across U.S.: Numbers That Tell the Story
Here’s the breakdown of how Nimbus is gaining ground:
Stronger Binding to Cells
Lab studies indicate Nimbus binds to the ACE2 receptor—the same gateway other variants use—about 2.5× stronger, which means more efficient infections.
Rapid Rise in Samples
In parts of California and the Midwest, sequencing data showed NB.1.8.1 rising from 2.5% to over 50% of detected COVID cases within weeks. Nationally, it’s around 37% by early June.
Wastewater Surveillance
Monitoring of untreated wastewater—a reliable early indicator—shows a consistent 50% increase in viral load in several urban areas, hinting that actual cases might be higher than reported testing suggests.
What Does Nimbus Feel Like? Symptoms and Severity
The most unusual complaint? The “razor‑blade throat”—so painfully scratchy it feels like you’re swallowing glass. This has become the go-to descriptor on social platforms.
But not everyone gets that symptom. Here’s a typical profile:
- Fever and chills
- Dry cough or mild congestion
- Headache and fatigue
- Upper respiratory discomfort
- GI symptoms – nausea or diarrhea (in fewer cases)
Research and official health sources confirm that NB.1.8.1 does not increase hospitalization or death rates compared to Omicron. So while it’s more contagious, it’s not more dangerous—yet it’s still a nuisance.
Vaccines, Boosters, and Immunity: What You Need to Know
Here’s the updated vaccine scenario:
- Reduced antibody effectiveness – about 1.6‑fold lower against Nimbus.
- But real-world protection against severe disease remains intact, particularly thanks to booster doses.
- If your last booster was over 6 months ago, or if you had COVID in early 2024, it’s time to consider another booster, especially for high-risk groups.
Vaccine Timeline
- 2024–25 booster rollout includes updated shots targeting Omicron subvariants, which also work against NB.1.8.1.
- Questions about eligibility, availability, or side effects?
Practical Steps: What You Should Do
1. Keep an Eye on Symptoms
That razor‑blade throat? SusPECT it could be NB.1.8.1. Grab a test if you’re feeling scratchy, feverish, or fatigued. Home test results are accurate for detecting this variant.
2. Mask Up Indoors
You don’t need a full bubble—but a KN95 or N95 mask at airports, clinics, or crowded venues is smart. Masks reduce transmission and protect vulnerable people.
3. Stay Boosted
Got questions about booster timing or access? Contact your local clinic, Indian health service centers, or pharmacies. They’re offering updated shots tailored to Omicron subvariants.
4. Isolation and Testing
Test positive? Stay home for at least 5 days, and don’t return to group activities until symptoms resolve or a medical provider advises it.
5. Use Antivirals When Recommended
If you’re in a high-risk group (like elders, immunocompromised people, or folks with chronic health issues), ask about Paxlovid—early treatment can reduce hospital admissions by up to 89%.
Risk Outlook: Will We Face a Summer Surge?
The risk remains low, but there are signs of an uptick:
- Hospital visits for respiratory symptoms have risen ~20% in some regions.
- Testing positivity and wastewater levels—early indicators of spread—are trending upward.
- Seasonal behaviors: more travel, beach outings, festivals—plenty of opportunities for infection.
Still, pandemic levels of strain and fear are gone. With vaccines, treatments, and more tools, we’re in a different phase: manageable, proactive, and community-centered.
Say Goodbye to Botox and Brain Fog—This Simple Daily Habit Could Change Everything
The Truth About Vegetable Milk—Why Scientists Say It’s Not as Healthy as You’ve Been Told
Breakthrough in Cholesterol and Cancer Research—Why This Discovery Has Doctors on Edge
A Note on Tribal Communities and Rural Areas
Tribal lands and rural areas often face health disparities: lower access to clinics, systemic underinvestment, and logistical challenges in vaccine distribution. Here’s how to uplift protection:
- Coordinate with local clinics and IHS partners to host clinic days or mobile vaccination clinics.
- Use community radio, Facebook pages, and local language messaging to spread awareness.
- Create isolation spaces or supportive services for elders and immunocompromised individuals to stay at home safely.
Your leadership can make a big difference—especially in carrying safe traditions and gathering celebrations forward this summer.